THE VACCINES
FAST FACTS
- Vaccines are now available from all area health departments; we recommend that everyone eligible get a COVID vaccination at this point.
- The Pfizer/BioNTech and Moderna vaccines are “mRNA” vaccines, which code for the inactive, non-infectious spike protein of the virus, tricking your immune system into fighting off these proteins and creating lasting immunity.
-
The Johnson & Johnson/Janssen vaccine is a modified adenovirus that has a bit of DNA coding for the coronavirus spike protein.
-
All of the vaccines given EUA or full FDA approval thus far are over 80% successful at eliminating severe or lethal COVID infections — including those caused by the Delta variant.
A QUICK NOTE ON NEW VACCINE TECHNOLOGY
mRNA vaccines have been in development since 1989. Initially we weren’t very good at making them, but science kept advancing. Moderna (notice it ends in “RNA”) was founded in 2010 to apply this science, and others like Pfizer did as well. Pfizer and Moderna were able to make a COVID vaccine almost immediately because all they had to do was put the mRNA sequence of the virus spike protein into their vaccine already in development, and voila!
We developed mRNA vaccines against MERS, SARS, and H1N1, none of which made it to the public — not because of safety, but because those germs fizzled out without needing a vaccine (unlike COVID). The SARS and MERS vaccines have 3 years of long-term safety data without major adverse events, and the H1N1 vaccine was developed in 6 months (a similar timeline to our current situation).
We’re not going to wade into politics, vaccine mistrust, or the history of systemic abuse of minorities by the medical establishment. Don’t get us wrong; all of that is very important in understanding the current situation, but the most important message we have is: trust the process. Trust the expert physicians advising the FDA and CDC, trust the science, and talk with your family and friends about their perceptions of the vaccine. Share this document or other quality information to those that want to learn more about the vaccine.
WADING THROUGH ALL THE INFORMATION OUT THERE ABOUT THE VACCINES
Speaking of trust and experts, generally speaking, when it comes to doing “research” about COVID vaccines:
- Our first recommendation is to double-check the source from which your information is coming. There is a painful amount of misinformation floating around, and while we want to be able to debunk each and every myth, the truth is that double-checking the reliability of the source is almost more important (and, frankly, more efficient).
- Finding a good source for your information is important not just in the realm of COVID and vaccines — it’s important for life! There are people out there (scientists, journalists, researchers, and epidemiologists) who are experts in this field.
- In order for us all to survive in our lives, we truly have to rely on experts to help us navigate complexities that just aren’t in our lane. For example, we rely on experts to build our roads and buildings (you wouldn’t hire just anyone to build your house, right? You’d hire a contractor and architect who know what they’re doing). We rely on expert engineers and manufacturers to build our smart phones (you’re not going to buy just any smart phone off the street — you buy one built by a company with a good reputation, right?). We rely on legal experts when we have to deal with the court system.
- Finding good, reliable experts makes it easier for you — for all of us — to get through complex information.
- Good sources for vaccine information:
- CDC.gov has guidance on COVID from a national perspective.
- Both KDHE (for Kansas) and MDHSS (for Missouri) have more local information about COVID and vaccines.
- The Children’s Hospital of Philadelphia has an excellent Vaccine Education Center for all sorts of questions about vaccines — from the ingredients to side effects, you can get a lot of your concerns addressed here.
- If you are bold enough to do your own research, PubMed, The New England Journal of Medicine, and The Journal of the American Medical Association all are great resources that publish studies related to COVID; these studies are what experts use to frame their recommendations, and the science is continually being updated and changing!
- Though newspapers and journalists are one step removed from the above primary sources of information (i.e. they quote the above resources when they do their reporting), they can often distill the complicated information above into digestible information. News outlets that generally do a good job of nonpartisan, well-researched reporting when it comes to health and science are:
- The Associated Press
- Reuters
- USA Today
- The Wall Street Journal
- National Public Radio
- The BBC
- (This list isn’t comprehensive! But it’s a good start.)
COMMON VACCINE QUESTIONS
- If I had COVID, should I get the vaccine?
- Yes. The immunity from infection is long lasting, likely less than a year (at best); we recommend vaccination regardless of prior infection.
- Should I get antibody testing before getting the vaccine?
- No. Similar to above, a positive antibody test does not necessarily mean one is immune, there are very frequent false negatives, and the antibodies tested may not be indicative of permanent immunity. The result of an antibody test should not dictate whether or not to get the vaccine.
- What about children, pregnant women, and the immunocompromised?
- Speaking generally, pregnant women and certain people who are immunocompromised should get the vaccine (but we welcome a conversation if you fall into this category and have questions). Children who are eligible should get the vaccine.
- Once I get the vaccine, can I stop wearing this mask?!?
- Not quite yet. Experts recommend continuing to wear a mask even after the vaccine, largely due to the seriousness of the Delta variant and the continued spread of COVID.
Please reach out if you have any questions!
The above was last updated September 8, 2021
TESTING & SELF-QUARANTINE
QUARANTINE
FOR THOSE WHO ARE NOT VACCINATED: If you are experiencing any symptoms whatsoever of COVID or have had prolonged contact with someone with confirmed COVID and you have not completed a COVID vaccine series, please self-quarantine, continue to practice good hand hygiene, and avoid spreading any illness to others; even if you get a negative test result after going through w/ one of the below tests, the CDC still recommends quarantining for 10 days after symptom onset or for 14 days after exposure to a COVID positive individual.
FOR THOSE WHO ARE FULLY VACCINATED: according to the CDC, people who are fully vaccinated do NOT need to quarantine after contact with someone who had COVID unless they have symptoms; however, fully vaccinated people should get tested 3-5 days after their exposure, even if they don’t have symptoms, and wear a mask until their test result is negative.
Updated September 9, 2021
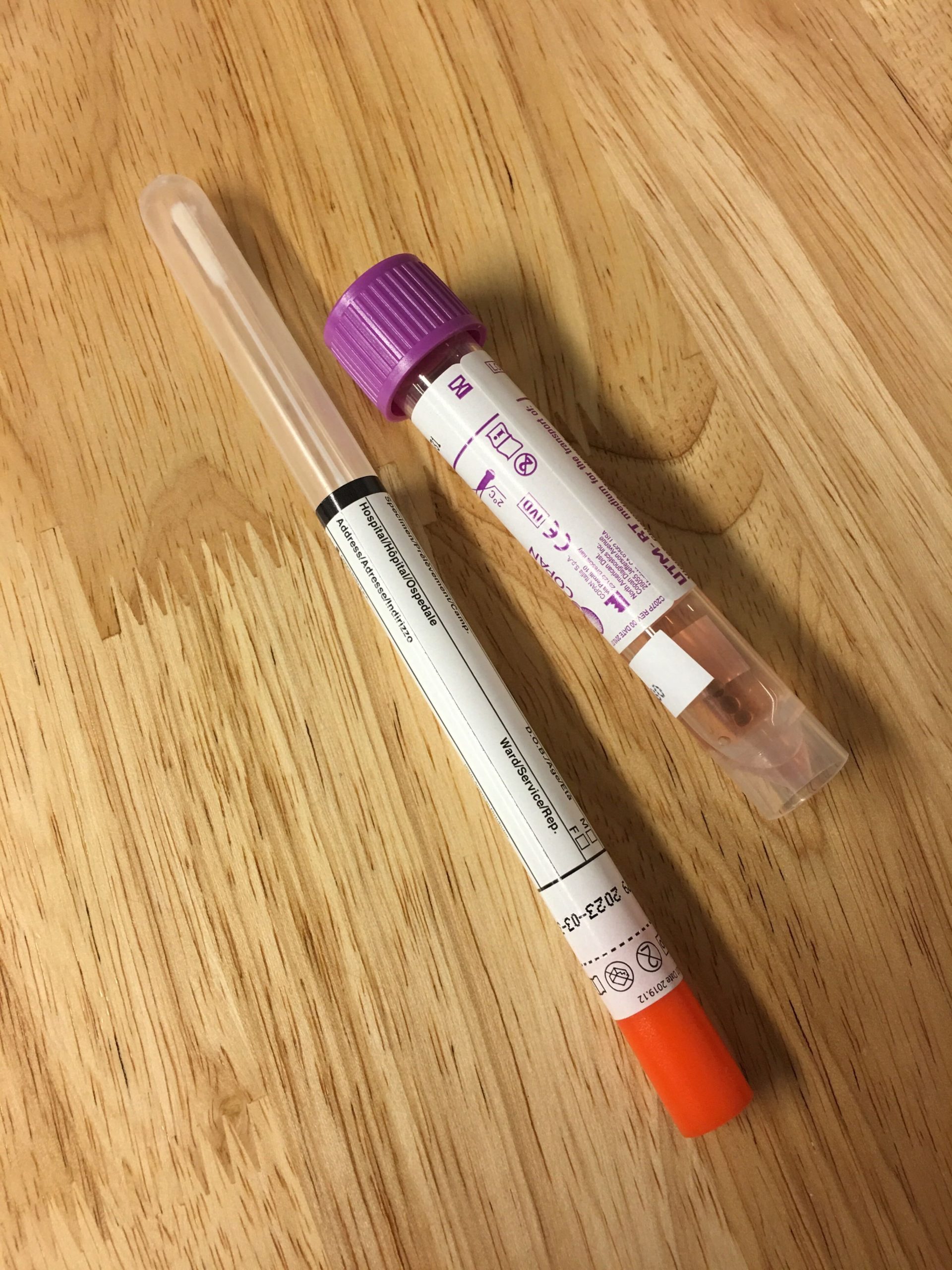
COVID TESTING
- We have limited rapid and send-out testing available here at the clinic — at a cost. Please reach out via info@kansascitydirectprimarycare.com or 913-730-0331 to inquire.
-
For no-cost testing, we recommend reaching out to your local health department!
- If you live in Kansas, check out the various health departments: Johnson County Health Department, Leavenworth County Health Department, & Wyandotte County Health Department.
- If you live in Missouri, check out the various local health departments: Cass County Health Department, Clay County Health Department, Jackson County Health Department, & Platte County Health Department.
- There are a few commercial entities that are providing testing as well (at a cost):
- Walmart is sending people to doineedacovid19test.com or MyQuestCOVIDTest.com depending on location.
- CVS
- Walgreens
- First Point Urgent Care (offering rapid antigen testing, not molecular PCR testing)
Updated September 8, 2021
CLINIC OPERATIONS
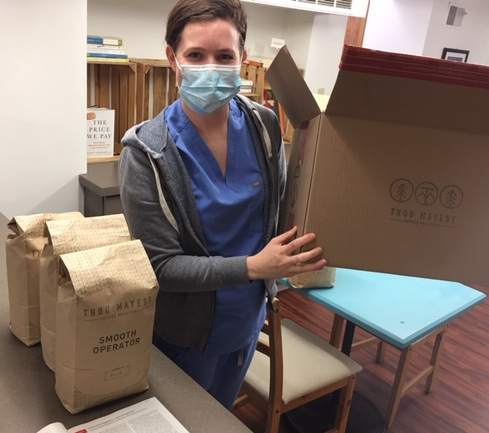
We are happy to announce that all staff and clinicians at KCDPC are fully vaccinated against COVID-19 — and we’re happy to hear more and more of you are getting vaccinated, too! This has allowed us to keep clinic operations as close to “normal” as possible. Here’s how things are going these days at the clinic:
- We are continuing to offer phone and virtual visits, just like we always have. For those who have been vaccinated, we are allowing for in-person visits as well.
- For those who have had an exposure to someone with COVID, who have symptoms concerning for COVID, or who have not received the full vaccine series for COVID, we may recommend a “car visit,” where we perform the elements of the visit in our parking lot while you are in your car. This is to help keep the spread of COVID to a minimum and to protect all of our patients.
- Feel free to email us with any concerns that pop up!
- We invite phone calls during normal business hours (we do our best to answer all of them — but sometimes we’re with a patient or on the other line; leave a message and we’ll call back)!
- Your clinician is available evenings and weekends (members only!) by following the voicemail prompts. Please let us know if this system ever gives you an error or doesn’t work (#techfailssometimes).
Updated September 8, 2021
NEWS & UPDATES
The biggest news currently revolves around the Delta variant. Here’s what we know about the Delta variant (information from the CDC at https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html ):
-
- The Delta variant is more contagious than prior strains of COVID — more than 2x as contagious.
- Some data suggest the Delta variant might cause more severe illness than previous variants in unvaccinated people.
- With regard to the Delta variant, unvaccinated people remain the greatest concern when it comes to risk of transmission of infection.
- Fully vaccinated people get COVID less often than unvaccinated people (“breakthrough infections”)
- Fully vaccinated people with the Delta variant breakthrough infections can spread the virus to others — however — vaccinated people appear to spread the virus for a shorter time.
- Masks: given what we know about the Delta variant, vaccine effectiveness, and current vaccine uptake, layered prevention strategies — like continuing to physically distance, wearing masks, etc. — are needed to reduce the transmission of this variant.
- Vaccines in the US are highly effective, including against the Delta variant.
- Get vaccinated! And if you’ve only had one of the two recommended doses, get your second dose!
Updated September 8, 2021